Abstract
Introduction. The role of minimal residual disease (MRD) has been confirmed as a clear prognostic factor by some big studies in Ph-positive acute lymphoblastic leukemia (Ph+ ALL) patients. The persistent MRD positivity may be indicative of the emergence of resistant mutations and TKI therapy should therefore be changed in these patients according to the sensitivity. Ph+ RALL protocol suggests that if a patient does not achieve the major molecular complete remission (MolCR) at day +70, Imatinib should be changed to Dasatinib for subsequent therapy. Could the change of Imatinib to Dasatinib in cases with MRD persistence at the end of induction improve the prognosis of the Ph+ ALL patients? It hasn't been described yet.
Aim. To evaluate the role MRD persistence at the end of induction (day +70) in Ph+ ALL patients treated by Ph+ RALL protocol.
Patients and treatment. From 2010 January to 2017 July, 36 new Ph+ ALL cases were diagnosed in 3 centers of the RALL-group (median age 35 years (17-68), m/f 19(53%)/17(47%), CNS disease=1, WBC> 30*109/l= 16(44%), bcr/abl transcript p190/p210/p190+210 21(59%)/8(22%)/7(19%)). All patients were treated according to RALL protocol with parallel administration of Imatinib. This protocol is based mainly on 600 mg Imatinib with prednisolone, VNCR, L-asp, followed by 6-MP and MTX. Imatinib had to be substituted by Dasatinib (140 mg) after non-achievement of MolCR on day 70 of treatment. MolCR was stated if bcr/abl chimeric transcript was <0,01% by PCR with 10-4 sensitivity. All patients were considered as candidates for allogeneic HSCT if HLA-identical donor was available. 16 pts (44%) underwent HSCT in the first-line therapy: 2 (12,5%) autologous, 4 (25%) matched related and 10 (62,5%) matched unrelated.
Results. Hematological complete remission (CR) was achieved in 32 (89%) of 36 pts (except two early deaths and 2 refractory cases). On day 70 MolCR was achieved in 18 (56%) of 32 pts. Death on therapy (within 3 months of induction/consolidation) was registered in 4 (11%) cases, in 2 patients of them after day 70th of the protocol in CR. The major issue is the non-relapsed mortality after unrelated allo-HSCT (n=3, aGVHD and severe infections, at a median +4 months after HSCT).
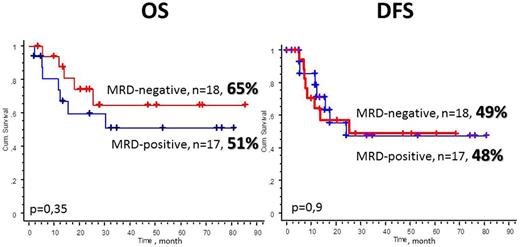
The 5-y overall survival (OS) and disease-free survival (DFS) for all 36 pts was 56% and 47%, respectively.
The 5-y OS was 65% vs 51% (p=0,35), and DFS was 49 vs 48% (p=0,9) in MRD-negative and MRD-positive patients on day 70th of the protocol (Picture). In a univariate analysis for Ph+ ALL patients the fulfilled of HSCT in the first-line therapy became statistically significant for DFS. The 5-y OS was 65% vs 48% (p=0,07), and DFS was 60% vs 32% (p=0,01) in transplanted vs non-transplanted patients by Kaplan-Meier analysis.
Conclusions. We didn't revealany difference in efficiency of the therapy in Ph+ RALL protocol according to the MRD status at the day 70. We attribute the absence of the effect of MRD status after induction on the results of treatment, to the shift to Dasatinib (140 mg) after non-achievement of MolCR on day 70. The performance of HSCT in the first-line therapy reliably improved the efficacy in Ph-positive ALL patients on RALL protocol.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal